
Provider Resources
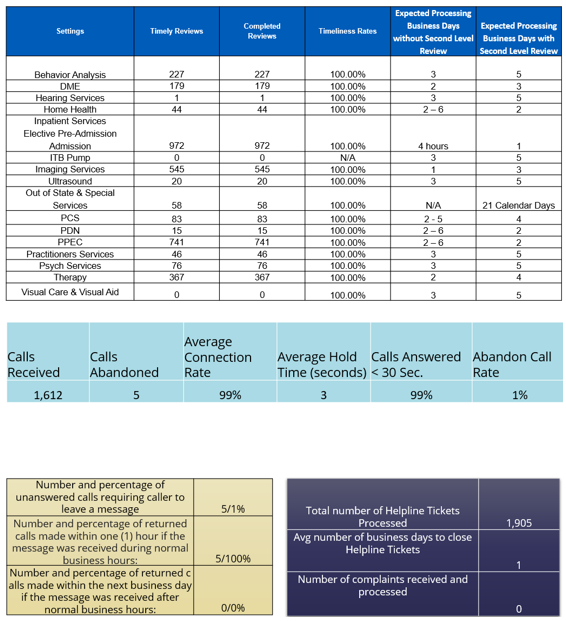
Performance Metrics
Register for a Training
If you are new to requesting authorization requests in eQSuite®, these webinars
will be an overview of requirements and expectations of submitting your request.
We will also have a live demonstration of entering an authorization request in eQSuite®.
How to Guides
Archived Bulletins
11/25/2020-FL Medicaid Health Care Alert
Electronic Visit Verification (EVV) Implementation (Click Here)
10/27/2020-FL Medicaid Health Care Alert
Electronic Visit Verification (EVV) Implementation (Click Here)
Submitting a Behavior Analysis Telemedicine Extension Request-9/3/2020
Click Here
Submitting a Behavior Analysis COVID-19 PA Extension Request-5/29/2020
Instructions (Click Here)
COVID19 PA Extensions for Behavior Analysis Providers-7/22/2020
BA Telemedicine Services-BA Providers may request an extension of administrative authorization for Telemedicine Caregiver Training for up to 60 Calendar Days. Please continue to refer to the Instructions posted to fl.eqhs.com on how to submit your request. You will follow set A or B instructions for telemedicine extensions based off the dates on the most recent telemedicine administrative approval.
BA Direct Services-Providers may request an extension of BA Direct Services for up to 90 Calendar Days. Please continue to refer to the instructions posted on our website on how to submit your request.
Administrative Authorizations for Hospital Transfers
(Instructions Click Here)
Administrative COVID-19 Authorizations
(Instructions Click Here)
Prior Authorization Requirements Update
Click Here
Florida Medicaid Prior Authorization Reinstatement
Click Here
Manually Priced Durable Medical Equipment and Medical Supplies During COVID-19
DME COVID 4-2-20
New Centralized Website for Agency Issued COVID 19-Alerts
http://ahca.myflorida.com/covid-19_alerts.shtml
Medicaid Coverage of Services During the State of Emergency Related to COVID-19
FL Medicaid Health Care Alert-COVID-19
Behavior Analysis Services – Multidisciplinary Team and Comprehensive Diagnostic Evaluation Updates 11/4/19
FL Medicaid Health Care Alert (Click Here)
Behavior Analysis Services-Effective Immediately 9/19/19
Clarification for CDE Requirements for all BA Services.
FL Medicaid Health Care Alert (Click Here)
October 13, 2020:Behavior Analysis Authorization Requests
10.31.2020 Eligibility Instructions
eQHealth Solutions is pleased to announce that starting 9/23/19 BA providers located in MDT Regions 4&7 will now have the option to submit your authorization request in eQSuite®. If you have any questions please sign up for our Webinar scheduled for Monday September 23, 2019 at 11:30 am Est.
BA MDT Provider Bulletin (Click Here)
Hurricane Dorian Update:
Hurricane Dorian Provider Alert from the Agency For Health Care Administration:
FL Medicaid Health Care Alert-Hurricane Dorian
8/30/19
Due to the anticipated arrival and projected impact of Hurricane Dorian. eQHealth Solutions under approval of AHCA is waiving prior authorization requirements for life sustaining care services effective immediately through 9/13/19. We will continue to provide updates as Hurricane Dorian reaches landfall.
8/29/19
eQHealth Solutions has begun preparing for the impending threat of Hurricane Dorian. Currently, we are fully operational. We will closely monitor the FL State of Emergency Declarations and will continue to provide updates as evacuations occur and Hurricane Dorian reaches landfall.
Attention Behavior Analysis MDT Providers
This is a reminder that a Diagnostic Evaluation or an In-depth Assessment is required with your submission for BA Services. An administrative extension of services can only be applied If the recipient is currently authorized and receiving services and needs additional time to complete the assessment. Please see page 8 of our training presentation.
Behavior Analysis Training Webinars
eQHealth Solutions is excited to announce and welcomes BA providers to attend our continued webinar training series. Our training session topics will review “How to avoid Pends” and “Focus versus Comprehensive Treatment”. Our goal is to improve communication with the provider community and provide you with the tools you need to be successful with your authorization submissions.
A training calendar is posted on featuring the topic session and the registration information. The session is limited to 30 minutes, Sessions are scheduled during lunch and after regular business hours. If you are not able to attend a live training, sessions will be recorded and available on our website.
Please do not hesitate to contact us if you have any questions or concerns.
Behavior Analysis MDT Webinars
eQHealth Solutions is excited to announce and welcomes BA providers to attend our continued webinar training series. Our training session topics will review “How to avoid Pends” and “Focus versus Comprehensive Treatment”. Our goal is to improve communication with the provider community and provide you with the tools you need to be successful with your authorization submissions.
Our training sessions will be scheduled in Two Phases.
Phase 1 Topic Focus Areas:
- Behavior Plans
- Avoiding Pends
- Focus versus Comprehensive Treatment
Phase 2 Topic Focus Areas:
- MDT Process
- Provider Experience
- Parent Experience
A training calendar will be posted on our website fl.eqhs.org featuring the topic sessions and the registration information. We can accommodate 100 attendees per session, and session is limited to 30 minutes, Session are scheduled during lunch and after regular business hours. If you are not able to attend a live training, sessions will be recorded and available on our website. A Spanish language recording will also be available.
We appreciate your understanding and cooperation during this implementation. Please do not hesitate to contact us if you have any questions or concerns.
Behavior Analysis Providers
Provider Alert from the Agency For Health Care Administration:
Public Meeting for Proposed Behavior Analysis Changes
The Agency will host the first public meeting in a series of statewide meetings to introduce proposed changes to behavior analysis services covered under the Florida Medicaid program. Changes are being made to ensure children receive the right service, at the right time, and by the right provider.
The Agency is proposing to implement changes related to provider enrollment, service authorization, electronic visit verification, and payment of behavior analysis services over the next several months, with full implementation by July 2019.
The meeting will take place on Friday, March 29, 2019, from 10:30 – 11:30am EDT, at:
Agency for Health Care Administration
2727 Mahan Drive
Building 2
Tallahassee, Florida 32308
There will not be a phone call-in number available however, future statewide public meetings will take place and be noticed to providers.
Public Meeting for Proposed Behavior Analysis Changes (Click Here)
Attention All Hospital Providers:
As part of eQHealth Solutions’ contract with the Florida Agency for Health Care Administration (the Agency), eQHealth Solutions is required to annually review the utilization plans for all Medicaid participating hospitals to ensure compliance with the Code of Federal Regulations Title 42 Part 456 (Utilization Control §456.60–§456.145). Please be aware that hospitals must adhere to the submission timelines provided by eQHealth Solutions, which reflect the Agency’s guidelines.
• ALL 2019 UR PLANS MUST BE SUBMITTED NO LATER THAN JUNE 15th, 2019.
•INCLUDE YOUR MEDICAID PROVIDER ID # ON YOUR PLAN AND ALL HOSPITALS YOUR ID# COVERS.
•INCLUDE A CONTACT PERSON WITH THEIR EMAIL AND A PHONE NUMBER SHOULD WE HAVE ANY QUESTIONS.
We will review your submission, suggest any recommendations if needed and respond back with the results. If recommendations are made you will be afforded the opportunity to make any changes or corrections and resend the UR PLAN back in for review, the corrections must be received prior to the deadline.
Provider Alert from the Agency For Health Care Administration:
Important Upcoming Policy Change Reminder: New and Enhanced Self-Service Web Portal Features
FL Medicaid Policy Change Reminder (Click Here)
Behavior Analysis Providers:
Untimely Authorization Requests:
This is a reminder that Behavior Analysis Services are to be submitted as Prior Authorization. Any cases submitted for dates of service that are not current are considered untimely and will be cancelled. Please refer to our Phase 2 Provider Training, Page 40 and 43. You can also refer to AHCA’s Authorization Requirements Coverage Policy Bullet 2.0 via the following link FL Medicaid Authorization Requirements Policy Retrospective requests will be permissible if the recipient has Retroactive Medicaid eligibility or as specified in the policy.
2.0 Authorization Requirements
2.1 When to Request Authorization
- Providers must obtain authorization prior to rendering Florida Medicaid-covered services, except in an emergency, when:
- Specified in the service-specific coverage policy or the applicable Florida Medicaid fee schedule(s).
- Services will be performed out-of-state.
Thank you in advance for your cooperation.
Hurricane Michael Provider Alert from the Agency For Health Care Administration:
Hurricane Michael Provider Alert (Click Here)
Attention Home Health Providers:
UPDATE:
This is an update to the Home Health Services Electronic Visit Verification (EVV) Florida Medicaid Health Care Alert, Dated August 28, 2018. The details of this update are located via the link below.
Home Health Services (EVV) Update
Attention Behavior Analysis Service Providers:
When submitting prior authorization requests for BA services, providers must submit ALLmaterials to eQHealth as specified in Appendix 9.0 of the Behavior Analysis Services Coverage Policy. If eQHealth determines that the submission is incomplete or contains insufficient documentation to make a decision, it will inform the provider. The provider then has two business days to submit the remaining materials and/or documentation before the request is denied for lack of documentation. The provider can resubmit a complete authorization request at any time.
When requesting prior authorization for BA services, providers must submit one of the following types of comprehensive evaluations:
- Individualized Education Program (IEP)
- Evaluation by the recipient’s school district that has determined eligibility for special education
- Diagnostic evaluation conducted by one of the following:
- Developmental pediatrician licensed in accordance with Chapter 458, F.S. and certified by the American Board of Pediatrics
- Clinical psychologist licensed in accordance with Chapter 490, F.S.
- Child and adolescent psychiatrist licensed in accordance with Chapter 458, F.S. and certified or eligible for certification by the American Board of Psychiatry and Neurology
A complete request must include the recipient’s diagnostic evaluation report that contains clinical findings, recommendations, and a diagnosis. All submitted documentation must meet the requirements in accordance with Appendix 9.0 of the Behavior Analysis Services Coverage Policy (Rule 59G-4.125, F.A.C.).
FL Medicaid Behavior Analysis Services Information
Attention Behavior Analysis Service Providers:
In accordance with the Florida Medicaid Authorization Requirements Policy, eQHealth Solutions may request additional information as necessary to determine medical necessity.
When inadequate information is received that does not support the medical necessity of services, eQHealth notifies providers by requesting additional clinical information via eQSuites. Providers have (2) two business days to respond to the information request. If the information is not received within (2) two business days, the review will be denied for insufficient information.
If you submitted a request for prior authorization of behavior analysis services in the months of May or June and received a request from eQHealth for additional information and have not responded, please respond by July 20, 2018 with the requested information. If you do not respond by that date, eQHealth will begin to process denials for insufficient information.
Moving forward, requests for additional information that are not responded to by the provider within two business days, will be denied.
FL Medicaid Provider Alert (Click Here)
2018 Hospital UR Plan Submission
As part of eQHealth Solutions’ contract with the Florida Agency for Health Care Administration (the Agency), eQHealth Solutions is required to annually review the utilization plans for all Medicaid participating hospitals to ensure compliance with the Code of Federal Regulations Title 42 Part 456 (Utilization Control §456.60–§456.145). Please be aware that hospitals must adhere to the submission timelines provided by eQHealth Solutions, which reflect the Agency’s guidelines.
- ALL 2018 UR PLANS MUST BE SUBMITTED NO LATER THAN JUNE 15th, 2018.
- INCLUDE YOUR MEDICAID PROVIDER ID # ON YOUR PLAN AND ALL HOSPITALS YOUR ID# COVERS.
- INCLUDE A CONTACT PERSON WITH THEIR EMAIL AND A PHONE NUMBER SHOULD WE HAVE ANY QUESTIONS.
We will review your submission, suggest any recommendations if needed and respond back with the results. If recommendations are made you will be afforded the opportunity to make any changes or corrections and resend the UR PLAN back in for review, the corrections must be received prior to the deadline.
Attention PAC Waiver Providers
PAC Waiver has transitioned to Managed Care, effective January 1, 2018. For additional information, please visit the Agency’s website for information on Florida Medicaid’s PAC Waiver Changes :
Florida Medicaid PAC Waiver changes (Click Here)
Attention Home Health Providers
Home health administrators, directors of nursing, billing staff, as well as other designated individuals are encouraged to attend training on the Electronic Visit Verification (EVV) System.
Please visit the EVV Training page to sign up for training session date(s) and time(s) that best fits your schedule.
Hurricane Irma Update from eQHealth Solutions:
Given the recent events of Hurricane Irma, we would like to share that eQHealth Solutions is fully operational at this time.
We are working closely with AHCA to ensure that your needs are met, and we invite you to notify us immediately should you encounter any difficulties with our systems or processes. Please dial 855-444-3747 for Customer Support.
Our thoughts go out to those affected by Hurricane Irma, and we’re committed to providing you with the support you need during recovery
Hurricane Irma - Message from AHCA:
Click Here
Behavior Analysis Providers
We are inviting you to a webinar that will be held next week for Behavior Analysis providers. This webinar will be a review of eQSuite and how to enter a request for a modification. We will also have a Q&A session to go over any questions you may have. If you are not able to attend, we will be recording the session and posting it to our website for you to review at your convenience.
Date: Wednesday, May 9th, 2018 at 10:00am Est
Training Registration (Click Here)
We recently had our Phase 2 Training, if you were not able to attend you can watch the training via the link below.
Phase 2 Training (Click Here)
You can now view the FAQ's from the Phase 1 Webinar via the link below.
BA FAQs (Click Here)
Behavior Analysis-Phase 1
Reminder: If you need more units than the allowed amount in Phase 1, these requests must be faxed to us. The fax must clearly indicate that it is request for additional units. You can use the fax cover below.
BA fax coversheet-Click Here
Attention DME Providers-Recipients over the age of 21
When requesting authorization for a DME item please make sure you are referencing the Florida Medicaid Fee Schedule for the appropriate HCPCS Code. We have recently seen an increase of reviews submitted with the A9900 code. Please note A9900 is a -Misc DME Supply, accessory, and/or service component of another HCPCS Code .
(Example: briefs, diapers, protective underwear, pull-ons, liners, shields, guards, pads, wipes and undergarments)
You can reference the FL DME Imitations Handbook for additional information pp2-8.
PDN and PCS Providers
There have been recent changes to the Florida Medicaid Policy for Personal Care Services and Private Duty Nursing. You can find this policy by clicking on one of the links below.
FL Medicaid Coverage Policy for Personal Care Services
FL Medicaid Coverage Policy for PDN Services
One of the biggest changes is that you are now be able to request up to 180 days for all admission requests. Please make sure that if you are requesting 180 days that the prescription for services match your request.
Attention DME Providers
If you are entering a DME request please make sure you are referencing the Florida Medicaid Fee Schedule for Prior Authorization Requirements. If you do not have a copy of the Fee Schedule you can find them on our website on the following link.
Florida DME Fee Schedule
Prior Authorization numbers
When referencing the Fee Schedule if the code you are requesting has a “PA” this means the code requires prior authorization and once approved you will receive your authorization letter with a PA#.
If the code you are requesting only states “Medical Necessity” this means the code requires prior authorization however it does not require a PA #. This means a PA# will NOT generate when you receive your authorization letter. To avoid a denial on your claims make sure to include your authorization letter with your claim submission.
Submission Requirements for ADI and Outpatient Services
Untimely Authorization Requests
We wanted to remind you that all imaging and outpatient requests are required to be submitted as Prior Authorization. Until current we have been allowing and reviewing these cases. However, please refer to AHCA’s Authorization Requirements Coverage Policy. The only time Retrospective requests will be permissible is if the recipient has Retroactive Medicaid eligibility or as specified in the policy. Please note as of June 19th, 2017 we will be enforcing this policy and any cases with dates that have been submitted untimely will be cancelled.
Pended Reviews
We have recently seen an increase in “Pended” authorization requests for ADI. The current Coverage policy for ADI does not list specific documentation criteria. However AHCA’s Authorization Requirements Policy has specific criteria that we will be enforcing effective immediately.
Authorization Requirements Coverage Policy
To avoid a denial of your imaging request, please make sure to follow the submission requirements located under page 2 section 2.4 Submission Requirements. Failure to follow the stated requirements may result in denial of your request. Please make sure everyone within your organization who submits authorization requests are aware of these requirements.
Fair Hearing
As of March 1, 2017 The Fair Hearing Process has moved from being managed by DCF to now being managed by AHCA. The letters from eQHealth will be updated with the new information by the first of April until that time please be notified that the contact information for Fair Hearing is as follows:
You may ask for a fair hearing by contacting AHCA by telephone at (877)-254-1055, by fax at (239)-338-2642, in writing at, Agency for Health Care Administration Medicaid Hearing Unit P.O Box 60127 Ft.Myers, FL 33906 or by email at MedicaidHearingUnit@ahca.myflorida.com
Hospital UR Plans
The review process for 2017 UR PLANS has begun. We will review your submission, suggest any recommendations if needed and respond back with the results. If recommendations are made you will be afforded the opportunity to make any changes or corrections and resend the UR PLAN back in for review. Please note that the deadline for your submissions are May 31st 2017. Any submissions received after the deadline will not be reviewed. If you have any additional questions please contact urplans@eqhs.org
PACWAIVER FAXED REQUESTS
Please note that as of April 10th, 2017, eQHealth Solutions will no longer be accepting faxed or emailed requests for PACWAIVER requests. These reviews will need to be entered in by your organization online via eQSuite.
INPATIENT & IMAGING FAXED REQUESTS
Please note that on August 1st, 2016, eQHealth Solutions will no longer be accepting faxed in inpatient or advanced diagnostic imaging requests. These reviews will need to be entered in by your organization or the respective provider via eQSuite online.
MULTISPECIALTY FAXED REQUESTS
Please note that as of October 15, 2016, eQHealth Solutions will no longer be accepting faxed in multispecialty requests. These reviews will need to be entered in by your organization or the respective provider via eQSuite online.
If you would like assistance regarding entering in review requests via eQsuite, please refer to our online User Guide for assistance. If you have questions, please contact Provider Outreach at PR@EQHS.ORG.